Introduction
- Main function of lungs = bring atmospheric air into contact with blood
- ventilation = moving gas in and out of the lungs
- respiration = moving O₂ and CO₂ between air and blood
- conducting airways = those airways that provide a pathway to the gas-exchange membrane of the lungs
- do not participate in gas exchange
- in transit → gas is warmed, humidified and filtered by the Upper Airways
Upper Airways
^646d68
- consists of the nose, oral cavity, pharynx and larynx
- larynx marks the separation of upper and lower airways
Nose
- function = filter and condition air
- more resistance than airflow through mouth
- most breath through their nose at rest
- swollen mucous membranes = high nasal resistance | exercise = rapid breathing
- both cases → switch to mouth breathing
- structures that increase airflow resistance in nose are necessary to filter and condition air
- Nasal cavity divided into two channels called nasal fossae
- done by cartilaginous anterior portion of the nasal septum
- Posterior nasal septum formed by the vomer and ethmoid bones
- Two nasal fossae lead posteriorly → common chamber called nasopharynx
- through opening called choanae
- three of them that are downward-sloping, scrolled-shaped bones
- project from lateral walls of nasal cavity toward the nasal septum
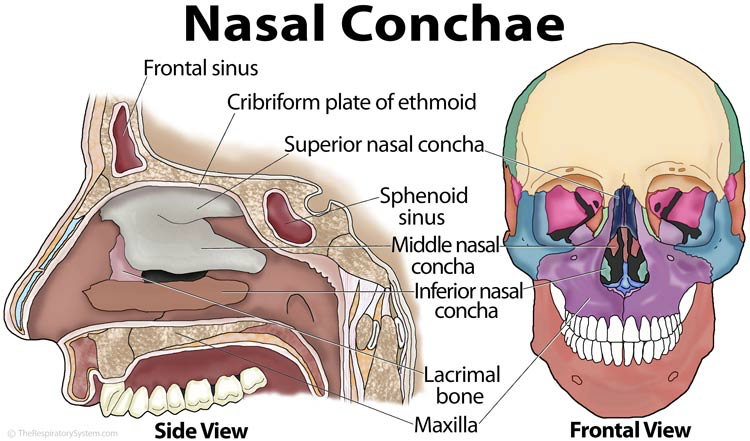
- They create three passages: superior meatus, middle meatus and inferior meatus
- Because they create turbulence of air, they are often called turbinates
- Increases surfaces area of the nasal cavity
- The maxilla forms the anterior 3/4ths of the nasal cavity floor → called hard palate
- cartilaginous structures form the posterior 1/4th → called soft palate
- During swallowing or coughing, the soft palate closes this posterior opening of the nasal cavity isolating the nasal cavity from the oral cavity (similar to the epiglottis in the pharynx)
- through opening called choanae
- The nasal septum is often deflected to one side or the other (L > R), making it more difficult to get a catheter or artificial airway in on that side.
- Immediately underneath the mucosa is an extensive capillary network thats connected to a deeper vessels with high-capacity
- Deep vessels can dilate or constrict and change the volume of blood that flows into the capillaries → altering the mucosa's thickness
- Capillaries have fenestrations that allow water transport to the epithelial surface
- not present in capillaries of lower airways
- Countercurrent blood flow and connections between arterial and venous vessels improve the ability of the nasal mucosa to adjust temperature and water content of inspired air
- To prevent mucosa's heat and vapor loss, the arterial vessels (warmer blood) run in parallel to the venous vessels (cooler blood) but in opposite directions
- Not present in airways below the larynx
- Main function of nose = humidification, heating and filtering of inspired air
- Inspired air passes over richly vascular epithelial surface (made even larger by turbinates) → increase in temperature and water content of air
- Turbinates disrupt the airstream and create swirling, chaotic flow → increases chances that tiny airborne particles will collide and adhere to sticky mucous layer
- Nasal secretions contain immunoglobulins and inflammatory cells = first defense against inspired microorganisms
- Nose can filter most particles larger than 5 micrometer in diameter
- Exhaled air cools as it leaves the nose and this causes water vapor to condense on its structures allowing subsequent inspired air to be humidified
- Inspired air passes over richly vascular epithelial surface (made even larger by turbinates) → increase in temperature and water content of air
- Sinuses
- Several empty airspaces within the skull and facial bones that connect to the nasal cavities
- Sinuses lined with mucus-secreting epithelium thats continuous with the nasal epithelium
- Mucus from sinuses drains into the nasal cavity through openings beneath the conchae
- 4 sinuses - frontal, ethmoid, sphenoid, maxillary
- Inflammation & infection in the sinuses → membrane swelling → impairing drainage & increases sinus pressure
Histology
- Anterior 1/3 of the nose → squamous, nonciliated epithelium
- Posterior 2/3 of the nose (including turbinates) → pseudostratified, ciliated, columnar epithelium interspersed with many mucus-secreting glands
- Mucus-secreting epithelium = respiratory mucosa
Pharynx
- Space behind the nasal cavities
- Extends down to larynx
- Nasopharynx = portion behind the nasal cavities that extends down to the soft palate
- Oropharynx = space behind the oral cavity,
- bound by soft palate above, base of the tongue below
- Laryngopharynx = space below the base of tongue and above the larynx
- In the posterior nasopharynx, inspired air quickly changes directions → particles collide and adhere to sticky mucous membrane
- In the nasopharynx and oropharynx there are lymphatic tissues -- pharyngeal (adenoid), palatine, and lingual tonsils
- Immunological defense against infectious agents
- Eustachian tubes (auditory tubes) connect middle ear with the nasopharynx
- allow pressure equalization between middle ear and atmosphere
- Inflammation and excessive mucous in the nasopharynx can block eustachian tubes → hinder pressure equalization → impairing hearing and causing pain (especially during abrupt pressure changes)
- Oropharynx and laryngopharynx (hypopharynx) acommodate food and air
- lined with nonciliated, stratified squamous epithelium
- Laryngopharynx separates digestive and respiratory tracts
- Pharyngeal reflex -- sensory component in CN IX (glossopharyngeal nerve); motor component in CN X (vagus nerve)
- responsible for gag and swallowing reflexes
- Pharyngeal reflex -- sensory component in CN IX (glossopharyngeal nerve); motor component in CN X (vagus nerve)
- Normal pharyngeal muscle tone prevents the base of the tongue from falling back and occluding the laryngopharynx even in those that are supine and asleep
- Deeply unconscious patients may relax their pharyngeal muscles enough to allow the base of the tongue to rest against the posterior wall of the pharynx occluding the upper airway → soft tissue obstruction = most common threat to upper airway patency
- Partial upper airway obstruction produces a low-pitched snoring sound as inspired air vibrates the base of the tongue against the posterior wall of the pharynx
Larynx
- Anatomy

- Cartilaginous, cylindrical structure
- Acts as a valve on top of the trachea
- Called voice box because it contains the vocal cords
- Main cartilage of the larynx = thyroid cartilage; sometimes called Adam's apple which is easily palpable in men
- Lies at the level of the fourth through sixth cervical vertebrae in men and located higher in women and children
- Top portion is a complex triangular box that is flat posteriorly and composed of an intricate network of cartilages, ligaments, and muscle
- Mucous membrane continuous with the pharynx lines the larynx
- Total of 9 cartilages -- 3 paired and 3 unpaired (epiglottis, thyroid, cricoid)
- Unpaired epiglottis = thin, flat, leaf shaped cartilage above the glottis
- Lower end of the epiglottis is attached to the thyroid cartilage
- Composed of elastic cartilage (the other laryngeal cartilages are hyaline cartilages)
- From this attachment, it slants upward and posteriorly to the base of the tongue
- Vascular mucous membrane covers the epiglottis → can become inflamed
- The lower base of the tongue is attached to the upper epiglottis by folds of mucous membrane forming a small space (the vallecula) between the epiglottis and tongue
- Vallecula = landmark used during insertion of a tube into the trachea
- Major function of larynx = preventing the lower airway from aspirating solids and liquids
- The epiglottis does not seal the airway during swallowing, instead the upper movement of the larynx toward the base of the tongue pushes the epiglottis downward, causing it to divert food away from the glottis and into the esophagus
- Thyroid cartilage is the largest of all laryngeal cartilages
- encloses the main cavity of the larynx anteriorly
- Lower epiglottis attaches just below the notch on its inside upper anterior surface
- Cricoid cartilage is just below the thryoid
- only complete ring of cartilage that encircles the airway in the larynx or trachea
- Cricothyroid ligament connects the cricoid cartilage and thyroid cartilage
- Cricoid limits the ET size that can pass through the larynx
- Inside the larynx, the vocal cords lie just above the cricoid cartilage
- Membranous space between cricoid and thyroid cartilage = cricothyroid membrane
- Arytenoid, corniculate and cuneiform = paired cartilages
- in the lumen of the larynx
- serve as attachments for ligaments and muscles
- Arytenoids = attachment points for vocal ligaments that stretch across the lumen of the larynx and attach to the thyroid cartilage
- Vocal folds consist of two pairs of membranes that protrude into the lumen (inner cavity) of the larynx from the lateral walls
- Composed of elastic fibers
- Lack blood vessels therefore they appear pearly white
- Vibration of vocal folds produces sound when air moves through the vibration
- Upper pair = false vocal cords
- Lower pair = true vocal cords -- only these play a part in vocalization
- form a triangular opening that is the entrance into the trachea
- called rima glottidis or glottis -- narrowest part of the adult larynx
- vocal cords ability to open and close the airway is essential for generating and releasing high pressure in the lung during a cough (extremely important lung defense mechanism)
- Artificial airways render cough ineffective because they prevent the vocal cords from sealing the airway
- Wider apart during quiet inspiration than expiration
- During deep inspiration, the vocal cords offer little airflow resistance
- Pitch of voice
- as length and tension of the vocal folds changes pitch varies
- tenser vocal folds = faster vibration = higher pitch
- Puberty
- Males' larynx enlarges during puberty → longer and thicker = slower vibration = deeper voice
- this change requires more control and until the male learns to control that, his voice will "crack"
- as length and tension of the vocal folds changes pitch varies
- Loudness of voice
- depends on the force with which the air rushes across the vocal folds
- What provides this force?
- muscles of the chest abdomen and back
- What provides this force?
- greater force → stronger vibration → louder sound
- whisper = no movement of vocal folds
- yelling = vocal folds vibrate vigorously
- depends on the force with which the air rushes across the vocal folds
- Valsalva maneuver → glottis closes, preventing exhalation → abdominal muscles contract → increase in intra-abdominal pressure
- Histology
- stratified squamous epithelium above the vocal cords
- pseudostratified columnar epithelium continuous with the tracheal mucosa below the vocal cords
- Branches of the tenth cranial (vagus) nerve provide motor innervation for all intrinsic muscles of the larynx through the recurrent laryngeal nerve
- Nerve passes downward around the aorta and returns upward to the larynx
- Partial or complete paralysis of the vocal cords is due to injury to this nerve
- Paralyzed vocal cords move to the midline increasing airway resistance
- Sensory innervation of the larynx = Vagus nerve except for the sensory nerves of the anterior surface of the epiglottis (supplied by CN IX)
- Laryngeal reflex = sensory and motor components of the vagus nerve -- vocal cords inside the larynx to close the tracheal opening (laryngospasm)
- occurs if anything except air enters the trachea
Lower Airways
- Divide in a pattern known as dichotomous branching -- each airway divides into two smaller daughter airways and each division gives rise to a new generation of airways
Trachea and Main Bronchi
- Trachea begins at the level of the 6th cervical vertebra and extends for about 11 cm to the 5th thoracic vertebra
- Divides there into right and left mainstem bronchi
- Division point = carina
- Inspired air becomes 100% saturated with water vapor and is warmed to body temperature after it passes through two or three subdivisions below the carina; the point at which this occurs = isothermic saturation boundary (ISB)
- Above ISB, temperature and humidity fluctuates, decreasing with inspiration and increasing with exhalation
- Below ISB, gas temperature and humidity remain constant at body temperature and 100% relative humidity
- Cold air, or mouth breathing moves the ISB deeper into the airways but never by more than a few generations
- Anterior portion of the trachea = 8 to 20 regularly spaced, rigid, horshoe-shaped cartilages
- Posterior portion of the trachea = flat, ligamentous membrane that contacts the esophagus
- Contains horizontally oriented smooth muscle, the trachealis
- Contraction of the trachealis pulls the ends of the horsehoe-shaped cartilages closer together → narrowing the trachea → more rigid
- Rigidity = important for preventing collapse from external pressure (especially coughing)
- Coughing exerts a collapsing force only on the part of the trachea inside the thoracic cavity about the 6th tracheal cartilage
- Above this level, trachea is outside the thorax and not influenced by intrathoracic pressure
- Rigidity = important for preventing collapse from external pressure (especially coughing)
- Right mainstem bronchus is straighter but larger in diameter and shorter than left mainstem
- Left mainstem bronchus is more acute angled, smaller in diameter and twice as long as the right mainstem
- The cartilage of the mainstem bronchi resembles the cartilage of the trachea initially except that cartilage completely surrounds the bronchi and the posterior membrane disappears
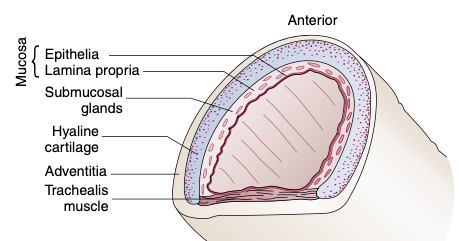
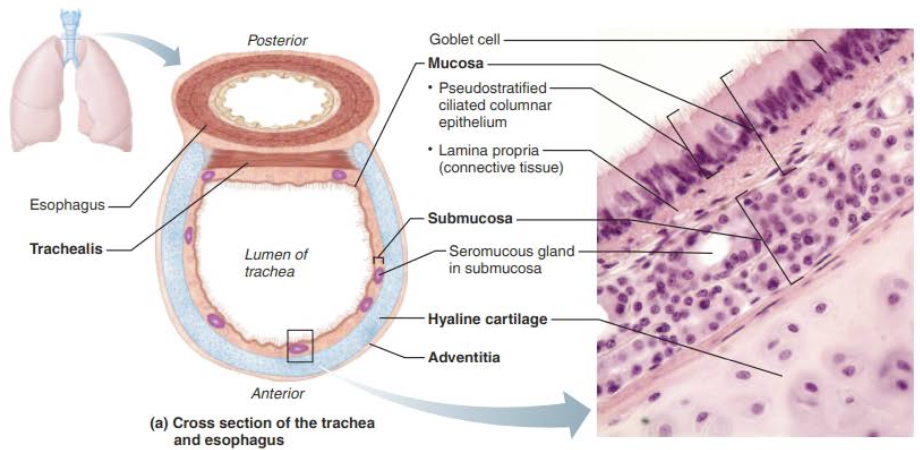
- Mucosa, submucosa and adventitia + hyaline cartilage
- Mucosa
- Goblet Cell-containing pseudostratified epithelium — occurs throughout most of the respiratory tract
- cilia on the mucosa propel debris-laden mucus toward the pharynx
- Smoker's Cough — smoking inhibits and destroys the cilia so the only way to get mucus up is by coughing
- the pseudostratified epithelium sits on a thick lamina propria
- Lamina Propria — rich supply of elastic fibers
- Submucosa
- Connective Tissue layer below the mucosa
- Contains seromucous glands
- produce mucus "sheets" within the trachea
- Supported by 16-20 C-shaped rings of hyaline cartilage
- Adventitia
- encases the hyaline cartilage
- outermost layer of connective tissue
- Mucosa
Conducting Airway Anatomy
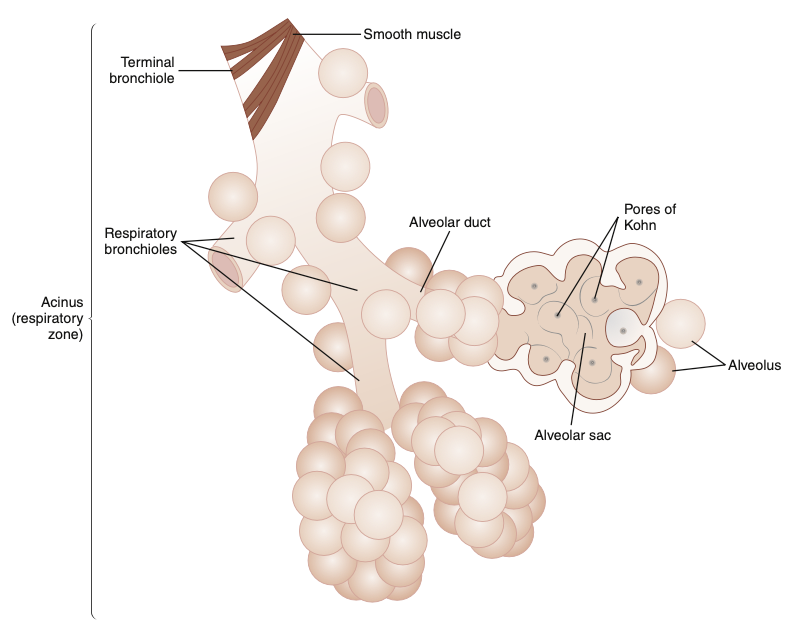
- Includes all airways down to the level just before alveoli first appear
- Do not participate in gas exchange only serve to conduct air to the alveoli
- Starting with the trachea, these undergo dichotomous branching until 23-27 subdivisions are formed
- Beyond the third generation of airway divisions, the bronchi enter the parenchyma, the essential supportive tissue composing the lung
- Elastic fibers of the parenchyma surround and attach to the airways
- their natural recoil forces act as tethers that hold the airway open during forceful exhalation
- These tethering forces also limit the degree to which smooth muscle contraction (bronchospasm) can narrow the airway
- Diseases that weaken parenchymal recoil forces make the airways prone to more severe narrowing or collapse, especially during exhalation.
- The natural elastic recoil forces of the lung are extremely important in keeping the small, noncartilaginous airways open
- Before the site at which alveoli first appear, the conducting airways subdivisions produce 1 million terminal tubes → massive increase in cross-sectional area of the airways
- This is a complex engineering design that allows uniform and rapid distribution of air through millions of tubes of various lengths and diameters without creating too much frictional resistance to air movement
- Airflow rate of 1 L per second (resting inspiration) requires a pressure difference of less than 2 cm H₂O between trachea and alveoli
- Volume of air in this conducting zone is relatively small so that the inhaled breath can contact the gas-exchange membrane
- About 150 mL (vs. total inhaled volume per breath is about 500 mL)
- Because the conducting airways do not participate in gas exchange, they are called anatomical dead space
- Bronchioles
- Airways less than 1 mm in diameter that contain no cartilage in their walls
- Patency depends on the tethering retractile forces of the lung's elastic parenchymal tissue
- Bronchial and bronchiolar smooth muscle is oriented in a circular, spiral fashion, facilitating airway narrowing when it contracts
- Strong smooth muscle contractions or spasms may nearly collapse the bronchioles especially if disease weakens the lung's opposing elastic tethering forces
- At the 9th or 12th generation, the terminal bronchioles divide to form several generations of respiratory bronchioles marking the beginning of the respiratory, or gas-exchange zone.
- Respiratory bronchioles = tubes containing thin, saclike pouches called alveoli in their walls
- Alveoli = gas-exchange membranes that separate air from pulmonary capillary blood
- Alveolar ducts open into blind terminal units called alveolar sacs and alveoli
- Airways beyond the terminal bronchiole are collectively called the acinus, i.e. each terminal bronchiole gives rise to an acinus
- Acinus = functional respiratory unit of the lung (i.e. all alveoli are contained in the acinus)
- Collateral air channels called pore of Kohn connect adjacent alveoli with one another
- The canals of Lambert connect terminal bronchioles and nearby alveoli
- These collateral air passages make it possible for the acinus supplied by a mucus-plugged bronchiole to receive ventilation from neighboring airways and alveoli
Sites of Airway Resistance
- Dichotomous branching creates an enormous increase in the total airway cross-sectional area → velocity of airflow is sharply reduced as inspired gas approaches alveoli
- Flow velocity is so low in small, distal airways that molecular diffusion is the dominant mechanism of ventilation beyond the terminal bronchioles
- Airways less than 2 mm in diameter account for only about 10% of the total resistance to airflow because of their large cross-sectional area.
- Resistance of a single terminal bronchiole > resistance of single lobar bronchus however the cross-sectional area of all terminal bronchioles >> cross-sectional area of a single lobar bronchus
- Therefore, upper airway resistance >> lower airway resistance
Conducting Airway Histology
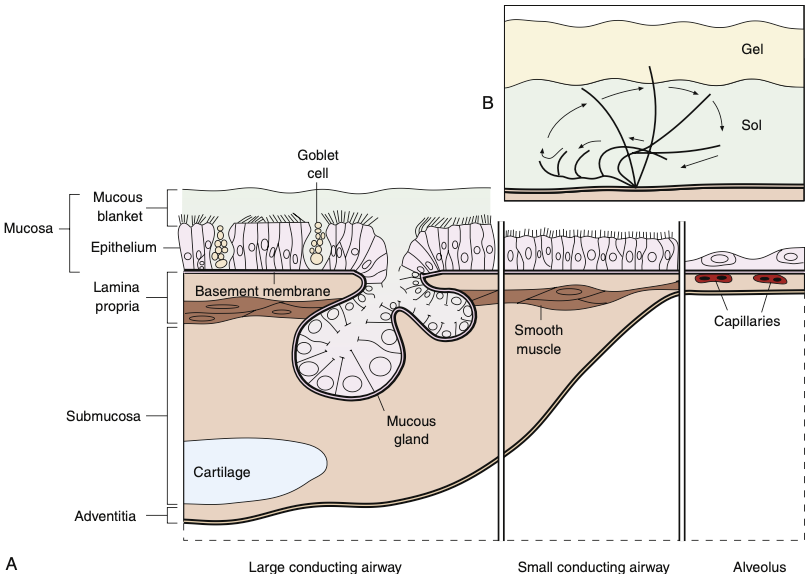
- Mimics that of the trachea
- Except as the conducting tubes become smaller, changes occur
- Support structure changes
- Cartilage rings (trachea) → irregular patches or plates of cartilage (bronchi) → no supportive cartilage (bronchioles)
- Bronchial Tree Walls contain elastic fibers
- Epithelium type changes
- Pseudostratified columnar (trachea) → simple columnar (bronchi) → simple cuboidal (terminal bronchiole) single layer
- Decrease of mucus-producing cells and cilia in bronchioles
- any debris found at or below the level of the bronchioles must be removed by macrophages
- Goblet cells decrease in # until they disappear at the level of the terminal bronchiole
- Club cells appear in smaller airways (mucous production and other functions)
- Mucus glands become progressively fewer in number more distally and absent in bronchioles
- Smooth Muscle Changes
- Trachea & Large bronchi — bands or spiral network
- Smaller bronchi and bronchioles — continuous layer of smooth muscle encircles the airway
- as airway size decreases distally → smooth muscle occupies larger portion of the total thickness of the airway wall
- maximal proportion of smooth muscle at level of terminal bronchiole
- Amount of smooth muscle increases
- the bronchioles have a complete layer of circular smooth muscle & no cartilage (would hinder constriction)
- This allows bronchioles to provide resistance to air passage
- Bronchial and Bronchiole Mucosa
- Appears to be several cells thick in the trachea and large bronchi however it's just the length of the columnar cells that makes it thick
- each cell rests on the basement membrane
- basement membrane contains collagen IV and laminin
- each cell rests on the basement membrane
- Along with the ciliated columnar cells, the mucosa also has basal cells, goblet cells in the bronchi and the bronchiole has the addition of club cells
- Goblet Cells
- Scattered between the ciliated columnar cells are mucin-secreting epithelial cells called goblet cells
- produce and discharge mucins into the airway lumen
- Mucins = large glucoproteins that once secreted to the lumen of the airway, expand physically and bind with water and other molecules to form a viscous gel
- Two predominant mucins — MUC5AC (produced primarily by GC; healthy persons = most abundent) and MUC5B (produced by cells in the submucosal glands)
- more prevalent in proximal airways → # dec as you move peripherally
- not present in terminal bronchioles
- Cigarette smoke causes all mucous cells to proliferate and spread into the small bronchioles where they are usually absent
- Tight Junctions
- between epithelial cells at the luminal surface, the epithelium prevents inhaled foreign material to the deeper levels of the airways through tight junctions
- inflammation can disrupt this barrier → antigens can penetrate
- Active Transport
- The epithelial cells allow active transport of ions most importantly chloride to provide a favorable ionic environment in the mucous layer
- Basal Cells
- Interspersed deep within the epithelium, abutting the basement membrane
- function — differentiate into and replenish more superficial cells of the mucosa (either the ciliated cells or the goblet cells)
- Club Cells
- Found in the more distal airways and terminal bronchioles
- function — same as basal cells (just named differently); also
- synthesis of immune molecules
- synthesis of small amounts of mucus and surfactant proteins
- metabolism of inhaled chemicals
- act as a progenitor for themselves and for ciliated cells
- Pulmonary Neuroendocrine Cell (Kulchitsky cell)
- found in the airway epithelium
- part of the amine precursor uptake and decarboxylation system
- capable of producing amine hormones (serotonin, dopamine, norepinephrine) & polypeptide products
- Cytoplasmic process extends to the luminal surface → ? sensing the composition of inspired gas → ? role in regional control of ventilation and perfusion
- These cell types in the airway mucosa are important for normal physiologic roles but also response to irritants and potential to become neoplastic
- Appears to be several cells thick in the trachea and large bronchi however it's just the length of the columnar cells that makes it thick
- Bronchial and Bronchiole Submucosa
- Two major components: Bronchial mucous glands & bronchial smooth muscle
- Mucus — 97% water + mucins + proteins (immunomodulators) + electrolytes + lipids + cellular debris
- Bronchial Mucus Glands
- located between bands of smooth muscle
- present in the trachea as well but most numerous in medium-sized bronchi
- base of the glands lined by mucous cells and serous cells
- connects to the airway lumen via ducts that are lined with ciliated cells
- The duct transports the secretions through the mucosa and discharges them into the airway lumen
- Primary mucin from mucus glands = MUC5B
- Serous cells
- Line the mucus gland
- Secrete proteoglycans and numerous antimicrobial substances involved in innate immunity
- may transform to goblet cells if chronically exposed to air pollutants
- Bronchial Smooth Muscle
- surrounds the mucous glands
- present from trachea down to the alveolar ducts
- Bronchial Fibrocartilaginous Layer
- similar function to the tracheal cartilage however the configuration varies unlike the trachea
- Adventitia
- connective tissue sheath that surround cartilaginous airways and blood vessels
- This sheath ends at the bronchioles → their airway walls are in direct contact with the lung parenchyma
Other Epithelial Cells
- Clara cells, found in the terminal and respiratory bronchioles, are non ciliated secretory cells that bulge upward into the airway lumen
- Normally the sole source of secretions at this level because mucous cells are absent
- Their secretions apparently also form part of the alveolar liquid lining.
- Injury to the epithelium at this level may cause the Clara cells to differentiate into ciliated or mucous cells
Mucociliary Clearance Mechanism
- Normal ciliary function and mucus composition are crucial for effective function of the mucociliary escalator
- lung's main method for removing microbes and inhaled particles that have gained access to the bronchial tree
- Approximately 100 mL of mucus is secreted per day in normal healthy people
- Mucus build up partially blocks or plugs airways and becomes a stagnant breeding ground for infectious microorganisms
- Abnormally thick mucus in the lower airways hinder ciliary motion and the efficiency of the mucociliary clearance mechanism
- Can be caused by decreased humidity in the airways due to water evaporating
Nonepithelial Cells in the Airway
- Inflammation of the lung causes various white blood cells such as eosinophils and neutrophils to enter the airways
- Mast cells are located on the epithelial surface of airways and in the airway walls near smooth muscle
- They have granules in their cytoplasm that contain preformed inflammatory agents (histamine, prostaglandins, leukotrienes, thromboxane, and platelet-activating factor)
- Release these granules when activated by a process called immune sensitization
- Inhaled irritants or antigens → plasma B cells → IgE → binds to specific receptor on mast cell surface → sensitizes mast cell → in the future exposure of antigen → cross linking of IgE → mast cell membrane rupture and release of granules
- Histamine -- causes the normally tight, impermeable cell wall junctions of airway epithelium to open → deep penetration → breaking down more mast cells → more vascular leakage, mucosal swelling, and bronchospasm
- Inflammation causes increased permeability of mucosal epithelium to water and causes mucosa to swell and smooth airway muscle to contract (bronchospasm)
Epithelial Chloride Channel Regulation and Secretion Viscosity
- Water movement into the airway lumen is an osmotic process influenced by epithelial cell membrane secretion of chloride ions
- Chloride ions are secreted into the airway through specialized epithelial channels (CFTR)
- Positively charged sodium ions follow this negatively changed chloride ions into the airway
- This ion secretion provides the osmotic force for water flow into the airway lumen and plays a major role in hydrating the mucus and facilitating normal ciliary function
- Various neurohormonal and pharmacological agents regulate epithelial chloride channels
- increase in cAMP → CFTR open → increased chloride secretion
- Increase cAMP → smooth airway muscle relaxation and bronchodilation
- β-adrenergic agonists → increase cAMP levels
- by doing so they also increase chloride secretion in normal airway cells accounting for the enhanced mucociliary clearance observed when β agonists are given
- increase in cAMP → CFTR open → increased chloride secretion
Epithelium-Derived Relaxing Factor
- Normal epithelium generates a substance that causes smooth muscle relaxation -- epithelial-derived relaxing factor (EpDRF)
- Modifies the responsiveness of airway smooth muscle to various stimuli
- Damaged or dysfunctional epithelial cells → do not produced EpDRF → response of smooth muscle to stimuli goes unchecked → hyperreactive airways → bronchospasm
- Damaged or dysfunctional epithelial cells may be partly responsible for the smooth airway muscle hyperreactivity characteristic of diseases such as asthma
Antiproteases in Lung Tissues and Airway Secretions
- Airway secretions and lung tissues contain inhibitors of proteolytic enzymes known as antiproteases
- In those with chronic airway inflammation, neutrophils invade the airways and release neutrophil elastase (NE) -- a powerful proteolytic enzyme
- Designed to destroy bacteria and other microorganisms that might be present in the airway
- When chronically present, it degrades elastin and collagen (major structural components of healthy lung)
- Healthy people have natural antiproteases in the blood, lung tissues, and secretions, the major one being α1 protease inhibitor (α1 antitrypsin)
- Another antiprotease in the lung is secretory leukoprotease inhibitor
- Both protect lung from NE released during episodes of airway inflammation
- In chronic airway inflammation, NE overwhelms the antiproteases and lung tissue damage occurs
- Balance of proteases and antiproteases is important for normal lung function